Cancer immunotherapy aims to mobilize the patient’s immune system and improve the activation of the antitumor immune response by changing the target from the tumor cells themselves. This aids in the immune cells’ ability to identify, target, and ultimately destroy the tumor cells.
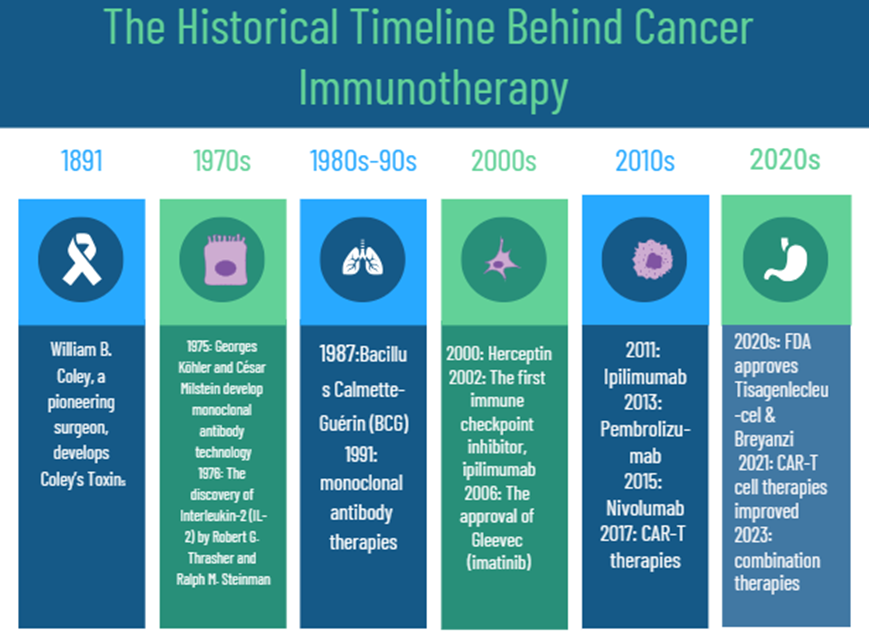
The Beginnings of Cancer Immunotherapy
Mechanisms of Cancer Immunotherapy
The human defense system encompasses numerous protective measures that shield the body against various dangers, including the proliferation of cancerous cells. Through diverse strategies, immune surveillance persistently detects and eliminates any abnormal tumor cells. Cancer immunotherapy has been hailed as the fourth cornerstone of tumor treatment, potentially exceeding the effectiveness of traditional interventions like surgery, radiation therapy, and chemotherapy. Notably, it was featured in Science’s 2013 compilation of the top ten scientific breakthroughs of the year. Zhang et al. categorized the mechanisms of cancer immune therapies into five primary types: adoptive cell transfer, cytokine treatments, cancer vaccines, oncolytic virus treatments, and immune checkpoint modulation.
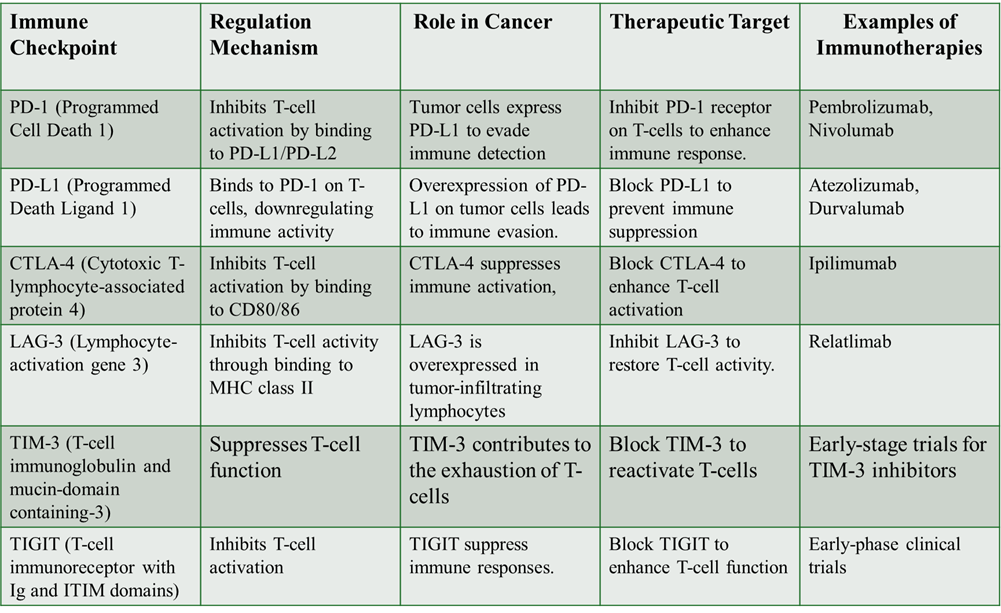
- Regulation of Immune Checkpoints
The objective of cancer treatment through immunological checkpoint modulation is to target proteins acting as negative regulators of immune responses to strengthen the immune system against malignant cells. Cancer cells can evade immune surveillance by expressing various immune checkpoint proteins, such as CD80/86, Gal9, and programmed cell death ligand 1 (PD-L1), which inhibit T-cell activation and multiplication. Immune checkpoint inhibitors and other therapies aimed at these immune checkpoint proteins have shown remarkable effectiveness in combating different cancer types. These drugs alleviate the suppression of T-cell activity by obstructing the interaction between immune checkpoint proteins and their ligands.
- Viro-Immunotherapy
In conjunction with immune checkpoint inhibitors and numerous other immunotherapeutic techniques, viruses have been extensively studied as the best therapy choice for a variety of cancer types. The goal of oncolytic virotherapy is to create highly selective genetically modified viruses that exclusively target cancer cells. These viruses identify cancer cells that express the specific chemicals and then lyse the cancer cells to infect and destroy them.
According to reports, vesicular stomatitis viruses (VSV) have several advantageous characteristics that support their application in immunotherapy, such as their innate tumor selectivity, quick replication kinetics, and ability to trigger a broad range of immune responses.
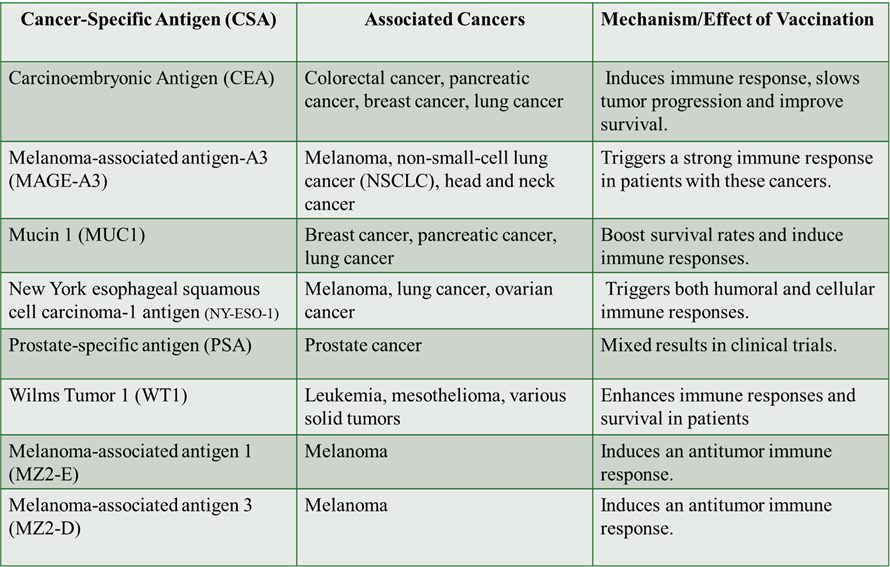
- Cancer Vaccines
Cancer-preventive vaccines aim to obstruct the development of cancer by targeting unique antigens specific to precancerous or early-stage malignant cells, or by addressing viruses known to trigger cancer. One approach that has exhibited potential as a viable therapeutic option involves the utilization of cancer-specific antigens (CSAs). CSAs are unique proteins or peptides present solely in cancer cells and are recognized by the immune system as foreign entities. Numerous CSAs have been explored, and they are currently being integrated into cancer vaccines to stimulate an immune response against malignant cells.
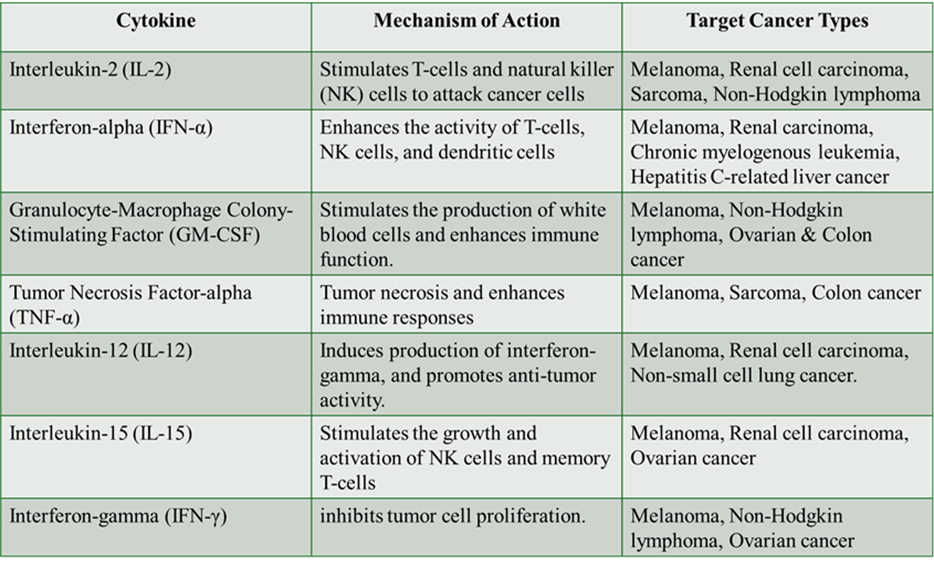
- Cytokine Therapies
In response to cellular stressors like infections, inflammation, and cancer, immune and non-immune cells secrete signaling molecules called cytokines that regulate cellular interactions. Interleukin-2 (IL-2) was first identified as a T-cell growth factor in 1976, marking the beginning of cytokine use in cancer therapy. When cultured with recombinant IL-2, inert lymphoid cells become lymphokine-activated killer (LAK) cells, capable of targeting tumor cells. Type I interferons (IFNs) were recognized over fifty years ago for their antiviral properties. Additionally, granulocyte-macrophage colony-stimulating factor (GM-CSF) promotes the differentiation of myeloid cells like neutrophils and macrophages in response to stress and cancer, also aiding in granulocyte recovery after chemotherapy.
- Adoptive Cell Transfer
To treat cancer, adoptive cell transfer (ACT) involves infusing immune cells, such as T cells, into a patient to detect and destroy cancer cells. T cells are often modified in the lab to enhance their ability to target cancer. A prominent type of ACT is CAR T-cell therapy, which modifies T cells to create chimeric antigen receptors (CARs) that latch onto specific proteins on cancer cells.
CAR T therapies offer significant advantages over traditional chemotherapy and radiation, selectively killing cancer cells while sparing healthy ones, which reduces toxicity. Additionally, CAR T cells can remain in the body for long periods, providing ongoing protection against cancer. However, CAR T-cell therapy is expensive due to the complex production process, potentially leading to delays in treatment for some patients.
Other Immune Therapies
T cells, B cells, and natural killer (NK) cells express the immune checkpoint protein Lag-3 (Lymphocyte Activation Gene 3), which regulates immune responses. Lag-3 has emerged as a potential target in cancer immunotherapy, with clinical trials investigating Lag-3 inhibitors, either alone or in combination with other treatments, showing promise for various cancers, including melanoma, lung cancer, and renal cell carcinoma.
To improve the delivery of immunomodulatory agents, nanoparticles and biomaterials are being used, enhancing pharmacokinetics and enabling targeted localization. Additionally, peptide-based materials are being explored to address therapeutic challenges by mimicking proteins with specialized immuno-regulatory functions.
References
- Dillman, R. O. (2011). Cancer immunotherapy. Cancer biotherapy & radiopharmaceuticals, 26(1), 1-64.
- Lesterhuis, W. J., Haanen, J. B., & Punt, C. J. (2011). Cancer immunotherapy–revisited. Nature reviews Drug discovery, 10(8), 591-600.
- Liu, C., Yang, M., Zhang, D., Chen, M., & Zhu, D. (2022). Clinical cancer immunotherapy: Current progress and prospects. Frontiers in immunology, 13, 961805.
- Zhu, S., Zhang, T., Zheng, L., Liu, H., Song, W., Liu, D., … & Pan, C. X. (2021). Combination strategies to maximize the benefits of cancer immunotherapy. Journal of hematology & oncology, 14(1), 156.
- Waldman, A. D., Fritz, J. M., & Lenardo, M. J. (2020). A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nature Reviews Immunology, 20(11), 651-668.

MPhil, PhD Microbiology
Follow me ⬇️



Post Comment